Have you ever felt so overwhelmed by emotions that you wished you could simply disappear? The feeling of being trapped in a spiral of pain and despair, wanting to escape the anguish, is a reality for many individuals struggling with self-harm. Fortunately, there’s a beacon of hope in the form of nursing care plans, designed to address this challenging situation and guide individuals towards healing and recovery. In this comprehensive guide, we’ll delve into the intricacies of nursing care plans for risk of self-harm, empowering you to understand, support, and advocate for those in need.
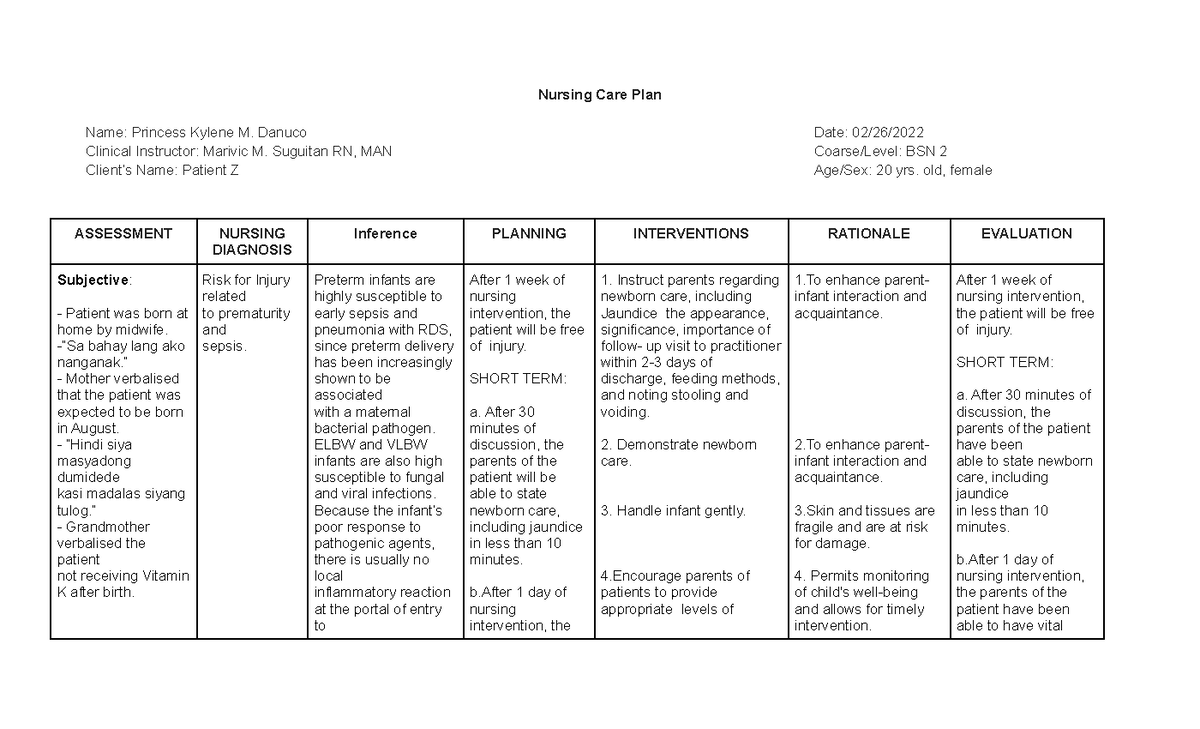
Image: www.studocu.com
Self-harm, a complex behavioral response to emotional distress, can manifest in various forms, ranging from cutting and burning to head-banging and hair pulling. Understanding the underlying reasons behind self-harm is the first step in effectively addressing the issue. It’s crucial to view self-harm not as a cry for attention but as a coping mechanism, albeit a maladaptive one, employed by individuals struggling to manage intense emotional experiences.
Understanding the Needs of Individuals at Risk of Self-Harm
Before jumping into the construction of a nursing care plan, let’s first understand the multifaceted needs of individuals at risk of self-harm. These needs are often intertwined and require a compassionate and holistic approach:
1. Emotional Regulation and Distress Tolerance:
Individuals who self-harm frequently lack effective coping skills to regulate their emotions, particularly intense emotions such as anger, sadness, or anxiety. They may find it challenging to tolerate emotional discomfort, leading them to seek immediate relief through self-harm.
2. Safety and Security:
The primary goal of any nursing care plan for self-harm is to ensure the safety and security of the individual. This involves creating a safe environment where self-harm behaviors are minimized and support is readily available.

Image: www.scribd.com
3. Communication and Trust:
Building a therapeutic relationship based on trust and open communication is paramount. Individuals at risk of self-harm may struggle to express their feelings openly, fearing judgment or rejection.
4. Understanding the Underlying Issues:
Self-harm is often a symptom of underlying mental health conditions such as depression, anxiety, trauma, or personality disorders. Identifying and addressing these underlying conditions is crucial for long-term recovery.
5. Building Coping Mechanisms:
Teaching individuals alternative and healthy coping mechanisms to manage their emotions and distress is vital. This might involve mindfulness techniques, relaxation exercises, journaling, or engaging in activities that bring them joy.
Developing a Nursing Care Plan for Risk of Self-Harm: A Step-by-Step Guide
Now, let’s dive into the process of developing a nursing care plan for risk of self-harm. Remember, this plan should be tailored to the individual’s specific needs and circumstances.
1. Assessment: The Foundation for Effective Care
The initial step involves a thorough assessment of the individual to gain a comprehensive understanding of their situation. This involves gathering information about:
- Suicidal ideation and intent: A direct assessment is crucial to determine the presence of active suicidal thoughts or plans.
- Self-harm behaviors: The frequency, intensity, and triggers of self-harm behavior should be explored.
- Underlying mental health conditions: Identifying any pre-existing or comorbid mental health conditions is essential.
- Coping mechanisms: Assess the individual’s current coping strategies and their effectiveness.
- Social support network: Understanding the individual’s support system and the level of reliance on it can inform the care plan.
- History of trauma or abuse: Past experiences of trauma or abuse can significantly influence self-harm behaviors.
2. Nursing Diagnoses: Defining the Problem
Based on the assessment findings, identify relevant nursing diagnoses that accurately describe the individual’s health status and needs. Some common nursing diagnoses for risk of self-harm include:
- Risk for Self-Directed Violence: This diagnosis applies when an individual exhibits behaviors or expressed intentions that suggest a potential for inflicting harm on themselves.
- Ineffective Coping: This diagnosis applies when an individual’s coping mechanisms are inadequate to manage their emotional distress, leading to self-harm or other maladaptive behaviors.
- Disturbed Thought Processes: This diagnosis is relevant when an individual’s thinking patterns are distorted
or disorganized.
3. Planning the Course of Action: Setting Goals
Once nursing diagnoses are established, the next critical step is to set realistic and achievable goals for the individual’s care. These goals should align with the nursing diagnoses and address the specific needs identified during the assessment.
- Safety: The primary goal is to prevent self-harm and ensure the individual’s safety.
- Emotional regulation: The goal is to enhance the individual’s ability to manage their emotions effectively.
- Coping skills: The aim is to equip the individual with alternative and healthy coping mechanisms to address their distress.
- Building a support network: The goal is to foster a sense of support and connection within the individual’s life.
4. Interventions: Putting the Plan into Action
The interventions outlined in the nursing care plan are the specific actions nurses will take to achieve the stated goals. These interventions should be evidence-based and tailored to the individual’s unique needs. Here are some examples:
- Safety interventions:
- Safety contract: A written agreement between the nurse and the individual outlining safe behaviors and strategies to avoid self-harm.
- Environmental modifications: Removing potentially dangerous objects from the individual’s environment.
- Close monitoring: Regular observation and check-ins to assess the individual’s mood and behavior.
- One-on-one supervision for high-risk individuals.
- Emotional regulation interventions:
- Teaching relaxation techniques (e.g., deep breathing, progressive muscle relaxation).
- Mindfulness exercises to increase awareness of thoughts, feelings, and sensations.
- Journaling: Encourage the individual to express their thoughts and feelings in a journal.
- Cognitive behavioral therapy (CBT) to identify and challenge negative thoughts and behaviors.
- Coping skills interventions:
- Identifying triggers: Helping the individual identify situations and emotions that trigger self-harm behaviors.
- Developing alternate responses to triggers: Teaching the individual to cope with triggers using healthy strategies (e.g., talking to a trusted person, engaging in physical activity).
- Teaching communication skills: Facilitating effective communication with others, including expressing feelings and needs.
- Support network interventions:
- Family education and support: Providing information to family members about self-harm and how to offer support.
- Group therapy: Connecting the individual with others who share similar experiences.
- Connecting with peer support groups: Connecting the individual to resources and support systems outside the hospital setting.
5. Evaluation: Measuring Progress and Adapting the Plan
The nursing care plan for risk of self-harm should be continuously evaluated to ensure its effectiveness and to make necessary adjustments along the way. This includes:
- Monitoring the individual’s behaviors: Observe for any changes in self-harm behaviors, emotional regulation, coping skills, and overall well-being.
- Assessing the individual’s perception of progress: Gather feedback from the individual about their experience with the care plan and their sense of improvement.
- Collaboration with other healthcare professionals: Work with psychiatrists, therapists, and other professionals to coordinate care and ensure consistency.
- Analyzing the effectiveness of interventions: Review the data collected and determine whether the interventions are effective in achieving the desired outcomes.
Expert Insights: A Beacon of Guidance
Throughout the care process, it’s crucial to draw upon expert insights from qualified mental health professionals. Here’s what some experts emphasize:
-
Building Trust and Empathy: Dr. Susan Miller, a renowned psychiatrist specializing in self-harm, underscores the importance of building a therapeutic relationship founded on trust and empathy. This involves listening attentively to the individual’s concerns, validating their feelings, and demonstrating genuine care.
-
Creating a Safe and Non-Judgmental Environment: “Individuals who self-harm need to feel safe and accepted,” says Dr. David Brown, a psychologist specializing in self-harm. Creating a non-judgmental environment free of shame and stigma is vital to encourage open communication and reduce the risk of self-harm behaviors.
-
Empowering Individuals for Long-Term Recovery: Dr. Emily Johnson, a nurse specializing in self-harm care, emphasizes the importance of equipping individuals with the tools and knowledge they need to manage their own long-term recovery. This involves teaching coping skills, promoting self-awareness, and fostering a sense of agency over their lives.
Actionable Tips for Supporting Individuals at Risk of Self-Harm
Here are some actionable steps you can take to support individuals at risk of self-harm, whether in your personal or professional life:
-
Recognize the Warning Signs: Pay attention to changes in mood, behavior, and appearance that might signal distress. Look for signs like social withdrawal, increased irritability, expressions of hopelessness, self-deprecating remarks, or sudden changes in eating or sleeping patterns.
-
Engage in Open Communication: Create a safe space for open and honest communication. Express concern without judgment and encourage the individual to share their thoughts and feelings.
-
Encourage Professional Help: Emphasize the importance of seeking professional help from a therapist or psychiatrist. Provide resources and support for accessing mental health services.
-
Be Patient and Understanding: Recovery from self-harm takes time and effort. Be patient, supportive, and understanding throughout the individual’s journey.
Nursing Care Plan Risk For Self Harm
Conclusion: Embracing Hope and Healing
Supporting individuals at risk of self-harm requires empathy, understanding, and a commitment to providing compassionate and effective care. The nursing care plan outlined in this guide is a roadmap to guide you through the process, ensuring the individual’s safety and fostering their overall well-being. Remember, self-harm is not a sign of weakness, but a symptom of underlying emotional distress. By understanding the individual’s needs, implementing evidence-based interventions, and collaborating with healthcare professionals, we can help individuals embark on a journey of healing and recovery.






