The moment a woman learns she’s pregnant, a wave of emotions washes over her – joy, anticipation, and maybe even a touch of fear. This fear often stems from the inherent vulnerability of the developing baby in the womb. As a nurse, I’ve witnessed firsthand the anxieties of expectant mothers, their faces etched with worry as they navigate the journey of pregnancy. One of the most pressing concerns for both mothers and healthcare professionals is the risk of fetal injury.

Image: www.scribd.com
It’s not just a theoretical possibility – it’s a real threat that requires vigilant monitoring and proactive care. This is where the nursing diagnosis of “Risk for Fetal Injury” comes into play. This diagnosis is a crucial tool that helps us identify, assess, and address potential dangers that could harm the developing fetus. Understanding this diagnosis and its associated interventions is essential for ensuring the safety and well-being of both mother and child.
Understanding the Risk for Fetal Injury Nursing Diagnosis
The nursing diagnosis of “Risk for Fetal Injury” is a clinical judgment concerning a vulnerable individual’s susceptibility to experiencing physical injury or damage to the developing fetus. This diagnosis is critical as it highlights the need for proactive and preventative measures to protect the fetus from potential harm.
It is characterized by the absence of overt injury but the presence of risk factors that increase the likelihood of fetal injury occurring. These risk factors can be categorized into several broad groups, including maternal health conditions, environmental hazards, lifestyle choices, and medical procedures.
Identifying Risk Factors
Recognizing the risk factors associated with fetal injury is the cornerstone of effective nursing care. Identifying these factors allows nurses to tailor interventions and provide individualized support. Some of the commonly encountered risk factors include:
- Maternal Health Conditions: Preeclampsia, diabetes, uncontrolled hypertension, infections like toxoplasmosis, and autoimmune disorders like lupus.
- Environmental Hazards: Exposure to environmental toxins, radiation, and secondhand smoke.
- Lifestyle Choices: Substance abuse (alcohol, drugs), smoking, and insufficient prenatal care.
- Medical Procedures: Invasive procedures like amniocentesis, chorionic villus sampling, and certain medications.
- Previous Pregnancies: History of premature birth, preterm labor, or fetal growth restriction.
- Age: Teenagers and women over 35 are at higher risk of complications.
Managing the Risk of Fetal Injury: A Collaborative Approach
Nursing care focused on preventing fetal injury requires a multidisciplinary approach. This involves close collaboration with other healthcare professionals, including physicians, midwives, and specialists. Nurses play a pivotal role in:
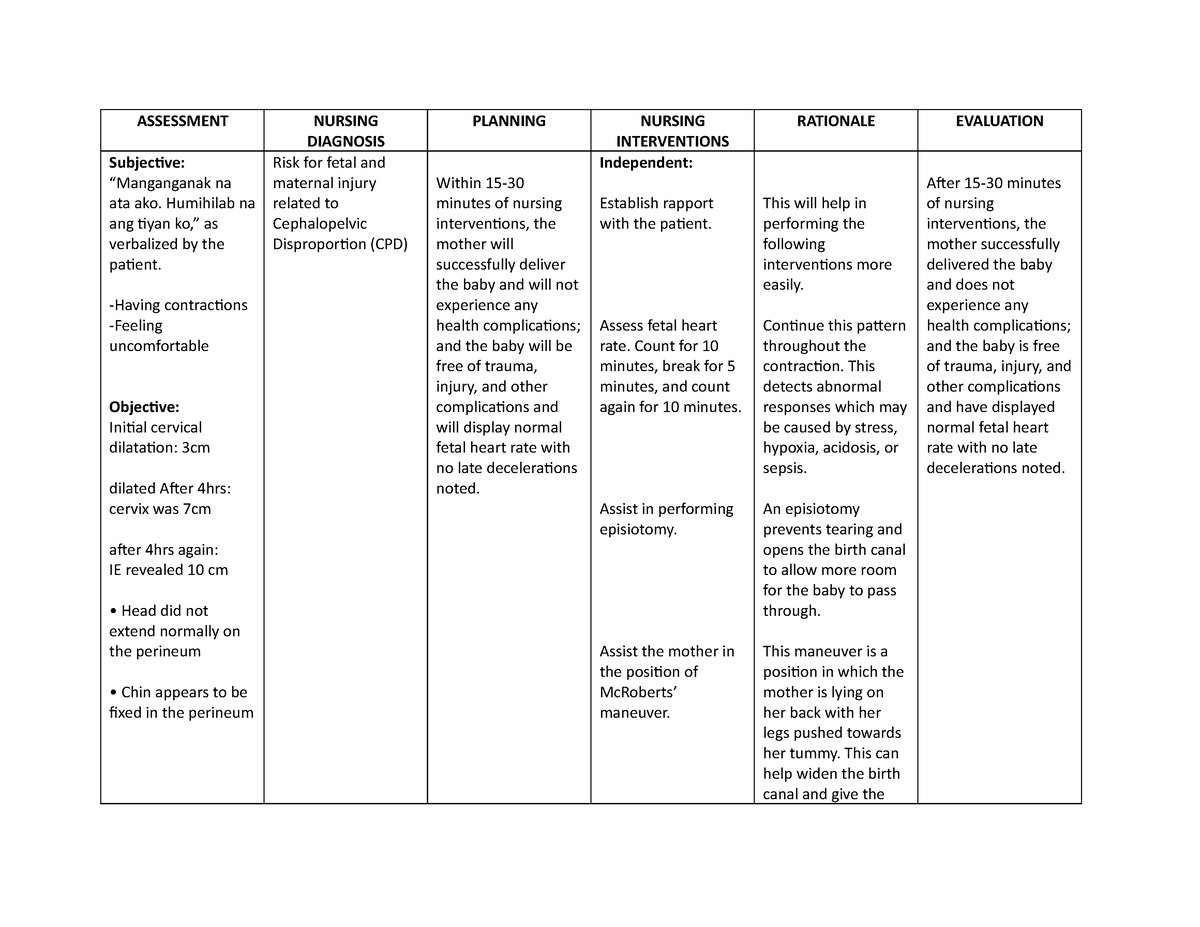
Image: www.studocu.com
Assessment and Monitoring
Nurses are the primary care providers who interact frequently with pregnant women. They are responsible for conducting thorough assessments to identify risk factors and monitor the mother and fetus closely. This includes taking vital signs, monitoring fetal heart rate, and assessing the mother’s general health status. Regular visits and consistent monitoring are essential for catching any potential issues early.
Education and Counseling
Nurses are vital educators who empower expectant mothers with knowledge. They provide essential information about healthy lifestyle choices, the importance of prenatal care, and the risks associated with potentially harmful behaviors. Counseling and support are crucial for addressing anxieties and promoting healthy coping mechanisms during pregnancy.
Implementation of Interventions
Based on the identified risks, nurses implement interventions to mitigate potential harm. These interventions may include:
- Lifestyle Modifications: Encouraging cessation of smoking and alcohol consumption, promoting healthy diet and exercise, and emphasizing the importance of regular prenatal care appointments.
- Medication Management: Administering prescribed medications for conditions like diabetes or high blood pressure, carefully assessing the potential risks and benefits of medications during pregnancy.
- Environmental Controls: Advising pregnant women to avoid exposure to known environmental hazards and minimizing exposure to secondhand smoke.
- Close Monitoring: Continuously monitoring the mother and fetus for signs of complications and promptly reporting any concerns to the physician.
Latest Trends and Developments
The field of maternal and fetal medicine is constantly evolving. Research is continually uncovering new insights into the causes and prevention of fetal injury. Some of the latest trends and developments include:
- Advanced Diagnostic Imaging: High-resolution fetal ultrasounds and other advanced imaging techniques allow for earlier detection of fetal abnormalities and potential risks.
- Personalized Medicine: Genetic testing and personalized medicine approaches are emerging that can predict individual susceptibility to certain pregnancy complications.
- Telemedicine: Virtual prenatal care and telehealth consultations are gaining popularity, offering increased accessibility and convenience for pregnant women.
Expert Tips and Advice
As a nurse, I’ve learned that the best care is individualized and proactive. Here’s some expert advice based on my experience:
- Early and Regular Prenatal Care: It’s never too early to begin prenatal care. Early detection allows for timely interventions and management of potential risks.
- Open Communication with Healthcare Providers: Don’t hesitate to ask questions and express any concerns you have about your health or the baby’s well-being.
- Healthy Lifestyle Choices: Maintaining a healthy diet, regular exercise, and avoiding harmful substances like alcohol and drugs are essential for a healthy pregnancy.
- Stress Management: Pregnancy can be stressful. Practice relaxation techniques like deep breathing, meditation, or yoga to manage stress levels.
Remember, a healthy pregnancy is a shared responsibility between the mother, her healthcare providers, and her support network. Being informed, proactive, and maintaining open communication are vital for a safe and successful pregnancy journey.
FAQs
What are the long-term consequences of fetal injury?
Fetal injury can have a range of long-term consequences, from developmental delays to permanent disabilities. The severity and impact vary depending on the nature and extent of the injury, the gestational age at which it occurred, and the specific health conditions involved.
What role does nutrition play in preventing fetal injury?
Proper nutrition is critical for the healthy development of the fetus. A balanced diet that includes essential vitamins, minerals, and nutrients is crucial for supporting fetal growth and preventing certain birth defects. Eating a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats is recommended.
How can I reduce my risk of fetal injury during pregnancy?
There are several steps expectant mothers can take to reduce the risk of fetal injury. These include:
- Avoiding alcohol and drug use.
- Cessation of smoking.
- Maintaining a healthy weight gain.
- Managing underlying medical conditions effectively.
- Receiving regular prenatal care.
Risk For Fetal Injury Nursing Diagnosis
Conclusion:
Risk for fetal injury is a complex nursing diagnosis that requires vigilant monitoring, collaborative care, and individualized interventions. By understanding the risk factors, implementing preventive measures, and fostering open communication, healthcare professionals and expectant mothers can work together to ensure a healthy and safe pregnancy journey. Are you interested in learning more about this important topic?






