Imagine yourself confined to a bed, unable to move freely. Even the simplest task, like reaching for a glass of water, becomes a struggle. This is the reality for many individuals facing impaired physical mobility, a condition impacting their quality of life and independence. It’s a complex challenge that requires skilled nursing care and a clear set of goals to guide patient recovery and rehabilitation.

Image: easystudyschool.blogspot.com
This article dives into the world of nursing goals for impaired physical mobility, outlining the crucial steps nurses take to support patients in regaining their movement and regaining control of their lives. From understanding the underlying causes of mobility limitations to implementing specific strategies and interventions, we’ll explore the intricacies of this essential nursing practice.
Understanding Impaired Physical Mobility: A Multifaceted Challenge
Impaired physical mobility refers to a limitation in a person’s ability to move their body independently. This can encompass a wide range of challenges, from difficulty walking or standing to complete immobility. The causes are equally diverse, ranging from:
- Musculoskeletal Conditions: Arthritis, osteoporosis, fractures, and muscle weakness can significantly impair movement.
- Neurological Conditions: Stroke, spinal cord injuries, multiple sclerosis, and cerebral palsy can disrupt nerve function and coordination, impacting mobility.
- Cardiopulmonary Conditions: Heart failure, chronic obstructive pulmonary disease (COPD), and other respiratory issues can limit stamina and endurance, affecting mobility.
- Cognitive Impairment: Conditions like dementia or delirium can affect a patient’s ability to understand and carry out instructions related to movement.
- Surgery and Trauma: Post-surgical recovery, traumatic injuries, and prolonged bed rest can result in muscle weakness and limited mobility.
The Vital Role of Nursing in Restoring Mobility
Nurses play a pivotal role in supporting patients with impaired physical mobility. Their expertise extends beyond simply ensuring patient safety and comfort. It’s about actively facilitating a patient’s journey towards regaining independence and improving their quality of life.
Establishing Nursing Goals: A Foundation for Success
Effective nursing care begins with establishing clear and measurable goals. These goals provide a roadmap for patient care and serve as benchmarks for progress. They should be:
- Specific: Clearly defined, focusing on a particular aspect of mobility.
- Measurable: Quantifiable, allowing nurses to track improvement.
- Attainable: Realistic, considering the patient’s current condition and capabilities.
- Relevant: Aligned with the patient’s needs and overall health goals.
- Time-Bound: Set within a specific timeframe, fostering a sense of progress.
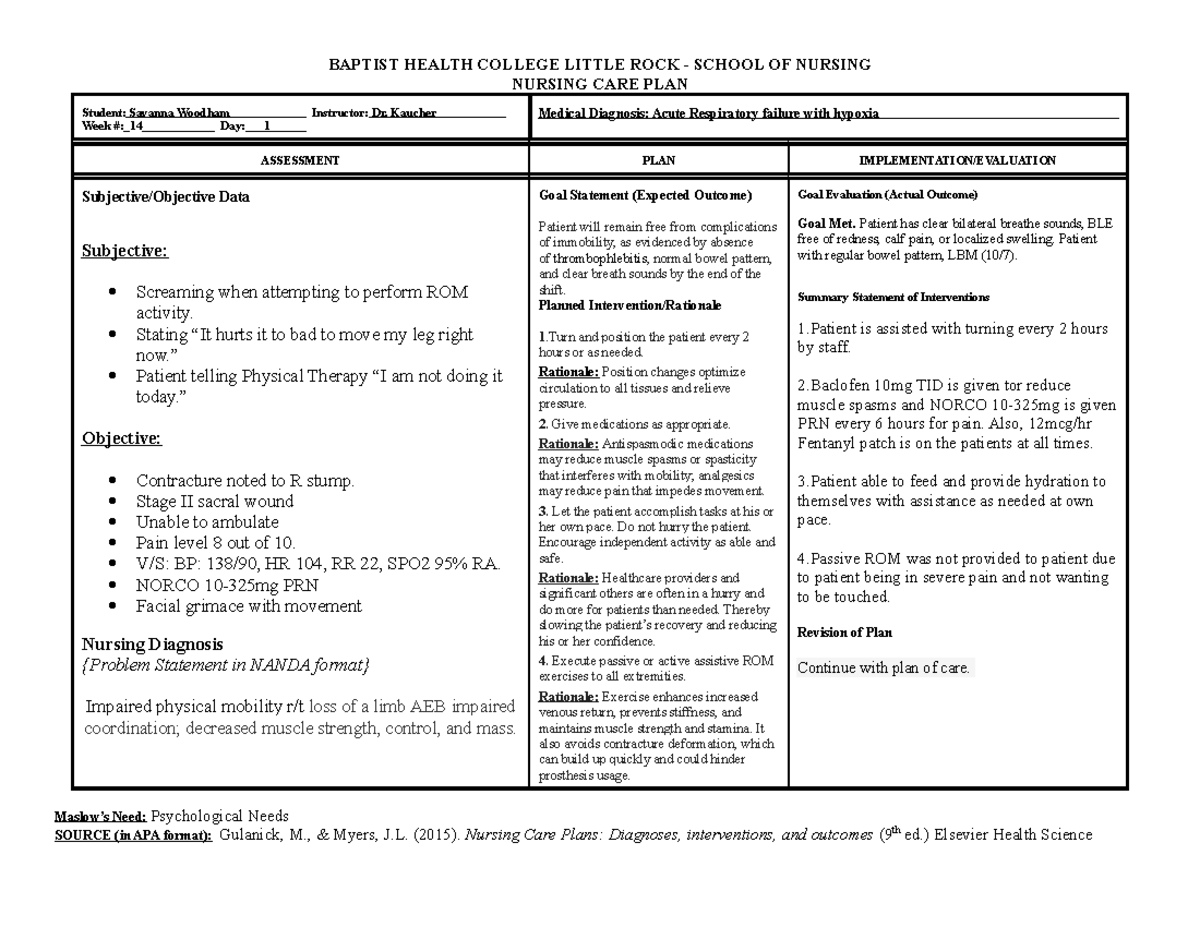
Image: www.studocu.com
Examples of Nursing Goals for Impaired Physical Mobility
Here are examples of nursing goals tailored to specific challenges associated with impaired physical mobility:
1. Enhancing Strength and Endurance:
- Goal: Patient will increase lower body strength to safely transfer from bed to chair by the end of the week.
- Intervention: Regular range-of-motion exercises, resistance training, and assistive devices like walkers or canes.
2. Promoting Gait Training and Balance:
- Goal: Patient will safely and independently walk 20 feet with minimal assistance by the end of the month.
- Intervention: Gait training with physical therapists, balance exercises, and the use of assistive devices like walkers or canes.
3. Preventing Contractures and Promoting Mobility:
- Goal: Patient will maintain full range of motion in both arms and legs by the end of the hospital stay.
- Intervention: Regular passive range-of-motion exercises, positioning aids, and the use of splints or braces to prevent joint stiffness.
4. Facilitating Safe Transfers and Positioning:
- Goal: Patient will be able to safely transfer from bed to chair with minimal assistance by the end of the week.
- Intervention: Using assistive devices like transfer boards, mechanical lifts, or slide sheets. Teaching the patient and caregivers safe transfer techniques.
5. Promoting Independent Activities of Daily Living (ADLs):
- Goal: Patient will be able to independently perform basic ADLs like dressing, bathing, and toileting by the end of the rehabilitation program.
- Intervention: Occupational therapy, adaptive equipment, and customized training to adapt to the patient’s limitations.
Strategies for Achieving Nursing Goals: A Comprehensive Approach
Nurses employ a multifaceted approach to achieve established goals, utilizing a combination of interventions based on the patient’s individual needs. These include:
1. Comprehensive Assessment:
A thorough assessment of the patient’s physical limitations, cognitive abilities, and medical history is crucial. This evaluation helps identify underlying factors contributing to impaired mobility and tailor interventions accordingly. Key areas assessed include:
- Muscle Strength and Range of Motion: Evaluating the strength and flexibility of the patient’s muscles and joints.
- Balance and Coordination: Assessing the patient’s ability to maintain balance and coordinate movements.
- Pain: Understanding the level of pain experienced by the patient and its impact on mobility.
- Functional Independence: Evaluating the patient’s ability to perform basic activities of daily living (ADLs) such as dressing, bathing, and toileting.
- Cognitive Status: Assessing the patient’s ability to comprehend instructions and follow directions related to movement and exercise.
2. Therapeutic Exercise Program:
Developing a personalized exercise program is essential for regaining strength, endurance, and mobility. It typically includes:
- Passive Range-of-Motion Exercises: Moving the patient’s joints through their full range of motion to maintain flexibility and prevent contractures.
- Active Assisted Range-of-Motion Exercises: Encouraging the patient to participate in exercises, with the nurse providing assistance as needed.
- Active Range-of-Motion Exercises: Encouraging the patient to actively move their joints through their full range of motion, building strength and coordination.
- Resistive Exercises: Using weights or resistance bands to strengthen muscles and improve mobility.
- Gait Training: Helping the patient to practice walking safely and effectively with appropriate assistive devices.
3. Assistive Devices and Adaptive Equipment:
Assistive devices can play a crucial role in promoting independence and reducing the risk of falls. Examples include:
- Cane and Walker: Providing support and stability for ambulation.
- Crutches: Assisting with weight-bearing and balance for patients unable to use their legs.
- Wheelchair: Enabling mobility for individuals with significant limitations.
- Transfer Boards: Facilitating safe transfers from bed to chair or other surfaces.
- Slide Sheets: Assisting with repositioning patients in bed with minimal effort.
- Adaptive Equipment: Modified utensils, grab bars, and raised toilet seats to facilitate independent daily activities.
4. Collaborative Care:
Nurses work in collaboration with a multidisciplinary team of healthcare professionals to address the multi-faceted needs of patients with impaired mobility. This includes:
- Physical Therapy: Developing individualized exercise programs to improve strength, endurance, balance, and coordination.
- Occupational Therapy: Assisting patients in adapting to their limitations and improving their ability to perform everyday tasks.
- Speech Therapy: Addressing communication challenges and providing strategies for safe and effective communication.
- Social Workers: Addressing socioeconomic factors influencing mobility, such as access to transportation or resources.
5. Patient Education and Empowerment:
Promoting patient understanding and involvement is key to successful rehabilitation. Nurses provide education on:
- Safe Transfer Techniques: Teaching patients and caregivers correct techniques for moving and safely transferring the patient.
- Exercise Program: Ensuring the patient understands how to perform exercises correctly and consistently.
- Assistive Devices: Explaining how to use devices effectively and safely.
- Fall Prevention Measures: Educating about common fall risks and strategies for avoiding them.
- Home Modifications: Discussing ways to make the home environment safer and more accessible for the individual with impaired mobility.
Challenges and Considerations:
While the goal is to restore mobility, the journey can be challenging for both patients and nurses. Considerations include:
- Pain Management: Effectively managing pain is crucial for patient cooperation and exercise adherence.
- Motivation and Engagement: Maintaining motivation for rehabilitation can be difficult, requiring ongoing encouragement and support.
- Safety Precautions: Implementing safety measures to prevent falls and complications during transfers or exercise is essential.
- Adapting to Limitations: The patient’s ability to adapt to new limitations and accept assistance may vary depending on their emotional state and coping skills.
The Impact of Impaired Physical Mobility: A Look Beyond Limitations
It’s essential to remember that impaired physical mobility is not solely a physical limitation. Its impact extends to the patient’s emotional, social, and mental well-being. It can lead to:
- Reduced Independence: Loss of independence in performing daily activities can lead to feelings of frustration, isolation, and depression.
- Social Isolation: Difficulty participating in social activities can result in decreased social interaction and feelings of loneliness.
- Decreased Quality of Life: Impaired mobility can significantly impact a patient’s ability to enjoy hobbies, pursue interests, and participate fully in life.
- Financial Strain: The need for assistive devices, home modifications, and ongoing care can create a financial burden for individuals and families.
Nursing Goal For Impaired Physical Mobility
Conclusion: Empowering Patients Through Nursing Care
Nursing goals for impaired physical mobility are not just about achieving a physical milestone. They’re about empowering patients to regain their independence, improve their quality of life, and participate fully in their communities. By combining expert knowledge, compassionate care, and a genuine commitment to patient well-being, nurses play a vital role in helping individuals overcome the challenges of impaired mobility and regain the ability to move with confidence and joy.
As you’ve learned, this field encompasses more than just exercise programs and assistive devices. It’s a holistic journey that requires understanding the patient’s unique needs, addressing their emotional well-being, and encouraging their participation in their own care. If you are facing the challenges of impaired mobility, remember that nurses are there to guide you, support you, and help you navigate this journey towards a brighter future.






