Imagine a world where a simple document, a seemingly mundane collection of words on paper, holds the key to someone’s journey to recovery from addiction. This is the power of progress notes within the world of substance abuse treatment. These notes aren’t just mere records; they’re a vital tool for understanding the intricate tapestry of an individual’s struggle and their progress towards reclaiming their life.
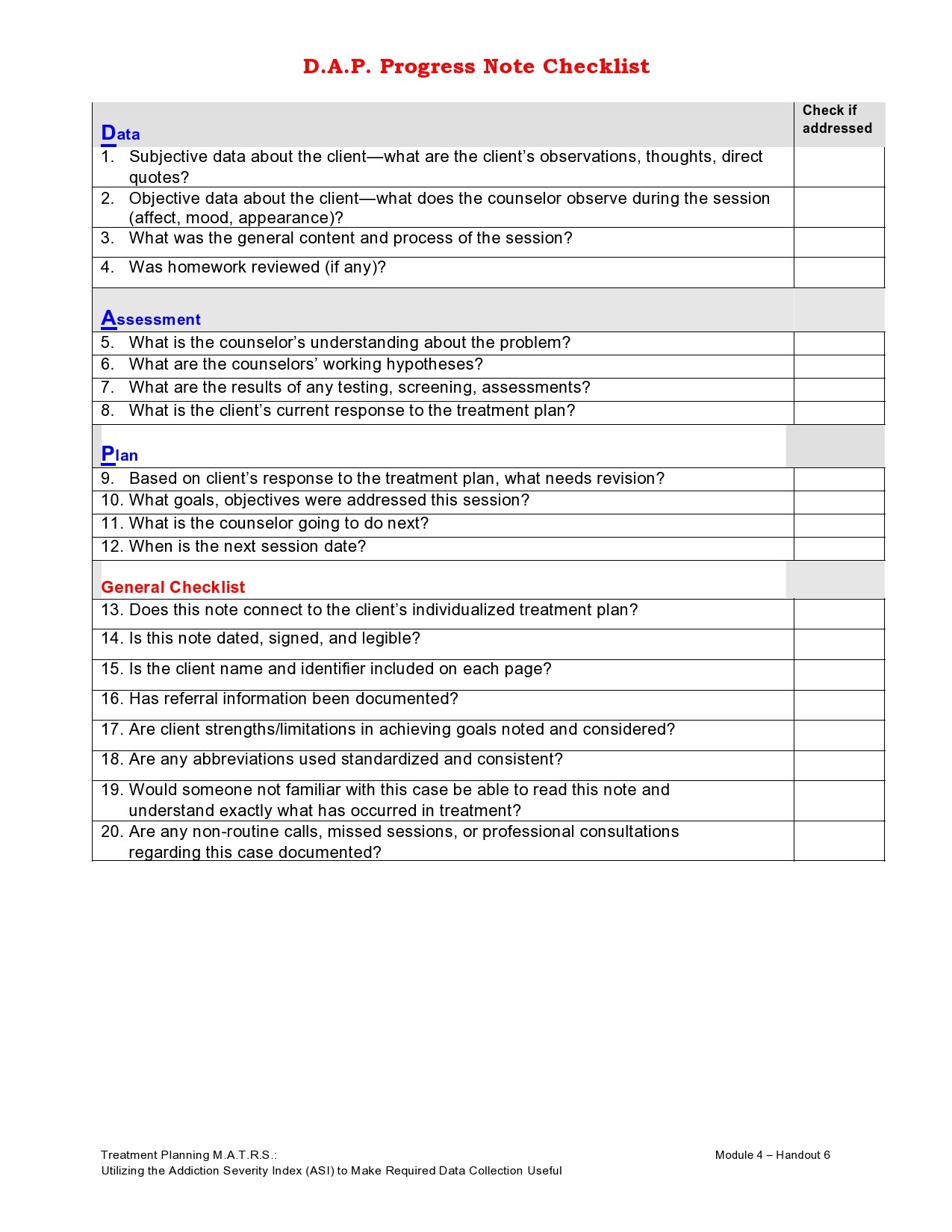
Image: www.vrogue.co
Substance abuse progress notes are the written accounts of a client’s journey through treatment. They are a confidential record of their experiences, their struggles, and their achievements, serving as a roadmap for clinicians and therapists to guide their care. This article delves into the world of these crucial notes, exploring their format, purpose, and the valuable insights they provide, illuminating the importance of this critical element in the recovery process.
Navigating the Landscape of Progress Notes: Structure and Content
Progress notes, often referred to as “SOAP notes,” follow a standardized format to ensure comprehensiveness and clarity. This structure helps clinicians quickly grasp the essence of a client’s situation and tailor their approach accordingly.
S – Subjective: The Client’s Perspective
This section captures the client’s personal experience, expressed through their own words. Here, they share their feelings, thoughts, and observations regarding their treatment, their triggers, and their progress.
Example: “Client reported feeling overwhelmed with anxiety today due to a stressful work deadline. She expressed frustration with her cravings for alcohol, stating that she felt like she was constantly on edge.”
O – Objective: The Observable Facts
This section presents the observable facts and data gathered about the client’s state. This could include:
- Vital Signs: Blood pressure, heart rate, body temperature
- Appearance: Physical presentation, hygiene, posture
- Behavior: Interactions, demeanor, mood changes
- Assessments: Results from standardized tests and questionnaires
- Medical Records: Documentation of any relevant physical or mental health conditions
Example: “Client appeared alert and oriented. She engaged actively in group therapy, maintaining eye contact and responding appropriately. Her speech was clear and coherent, and her mood was generally stable.”
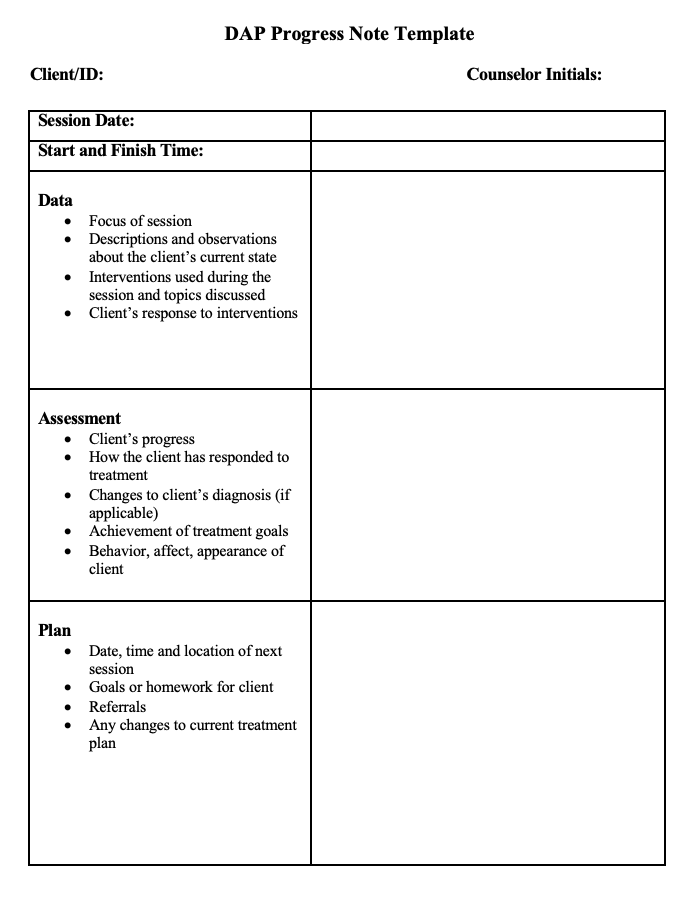
Image: template.mapadapalavra.ba.gov.br
A – Assessment: The Clinician’s Interpretation
This is where the clinician integrates the subjective and objective information, formulating a professional opinion about the client’s current state and treatment progress.
Example: “Client demonstrates an understanding of the triggers that lead to her substance use. Her anxiety level seems to be contributing significantly to her cravings. She expresses a strong motivation to stay sober, but her coping strategies need further development.”
P – Plan: The Roadmap to Continued Progress
This section outlines the clinician’s plan for the client’s continued care. It may include:
- Therapy Sessions: Frequency and type of therapy, including individual, group, or family therapy sessions
- Medication Management: Prescriptions or adjustments to existing medications
- Referral to Other Services: Recommendations for additional support, such as addiction support groups, counseling, or mental health services
- Follow-up appointments: Scheduling of future visits to monitor progress and adjust treatment as needed
Example: “Continue with individual therapy sessions twice a week. Encourage participation in group therapy sessions to develop coping strategies. Refer client to a support group for additional peer support.”
The Power of Observation: Insights from Progress Notes
Progress notes are more than just a record of a client’s journey; they contain a wealth of information that guides treatment decisions. Here are some important insights they provide:
- Identifying Patterns and Triggers: By analyzing trends in a client’s reports, clinicians can identify factors that contribute to cravings, relapse, or other challenges. This allows them to tailor treatment plans to address these root causes.
- Monitoring Progress and Setbacks: Tracking changes in a client’s mood, behavior, and physical well-being helps clinicians assess the effectiveness of treatment interventions. This allows them to make necessary adjustments to ensure optimal progress.
- Identifying Underlying Mental Health Issues: Clients struggling with substance abuse often have co-occurring mental health conditions. Progress notes provide valuable insights into these issues, facilitating appropriate interventions.
- Building a Comprehensive Picture: By documenting the client’s history, present struggles, and treatment response, progress notes create a holistic picture of their recovery journey. This information is essential for coordinating care with other healthcare professionals and ensuring a continuity of services.
Beyond the Paper Trail: The Collaborative Spirit of Progress Notes
Progress notes are not meant to be siloed documents. They serve as a foundation for collaboration and communication between healthcare providers involved in a client’s care.
- Fostering Communication: Sharing progress notes with other clinicians, including psychiatrists, primary care physicians, and social workers, ensures a coordinated and unified approach to treatment.
- Facilitating Transitions: When a client transitions from one setting to another, such as from inpatient rehabilitation to outpatient therapy, progress notes provide a seamless transfer of critical information.
- Building a Team Approach: By referencing the notes, clinicians can build a common understanding of the client’s challenges and successes, fostering a team spirit and ensuring consistent support throughout the recovery process.
Progress Notes: Shaping the Future of Recovery
The value of substance abuse progress notes lies in their ability to capture the complexities of addiction, document individual journeys, and guide a personalized path to recovery. They are more than just a formal record; they represent a powerful tool for understanding and treating substance abuse, empowering individuals to reclaim their lives and navigate a path toward lasting well-being.
As technology continues to advance, the application of progress notes is evolving. Electronic health records (EHRs) are increasingly utilized, streamlining information sharing, improving accessibility, and enhancing data analysis. This evolution allows for more precise and evidence-based treatment approaches, further emphasizing the pivotal role of progress notes in the future of addiction treatment.
Examples Of Progress Notes For Substance Abuse
The Legacy of Progress Notes: A Call to Action
The story of progress notes is a story of understanding, collaboration, and hope. They are a reminder that recovery is a continuous journey, filled with challenges and triumphs, and that each step, each observation, and each entry within these notes reflects the unwavering spirit of those striving to overcome addiction.
While this article has provided insights into the importance of progress notes in substance abuse treatment, it is just the beginning. The journey to recovery is a unique one for each individual, and it requires a commitment to ongoing learning and understanding. By engaging with resources, learning about the latest research, and sharing our voices, we can collectively contribute to the advancement of addiction treatment and empower those battling substance abuse to find their path to healing and lasting well-being.






